Volume 6 Issue 6 June 2016
According to the WHO, more than 450 million people worldwide suffer from mental illnesses and these conditions account for 14% of the global burden of disease. In other words, the prevalence of mental illnesses is very high. This translates to a lot of suffering. For instance, more than 8,00,000 deaths occur due to suicide every year and majority of them occur in developing countries like ours. Even these figures do not tell the complete story of burden of mental illness on the society. Consider the costs of destructive public health and safety implications, such as family disintegration, loss of employment, failure in school, domestic violence, child abuse, mental illnesses leading to poor physical health, substance abuse etc.
Contrast the magnitude of this burden to the fact that about 85% people suffering from mental health have no access to effective treatment. The financial resources needed to mitigate this situation are very modest. So why are we still struggling?
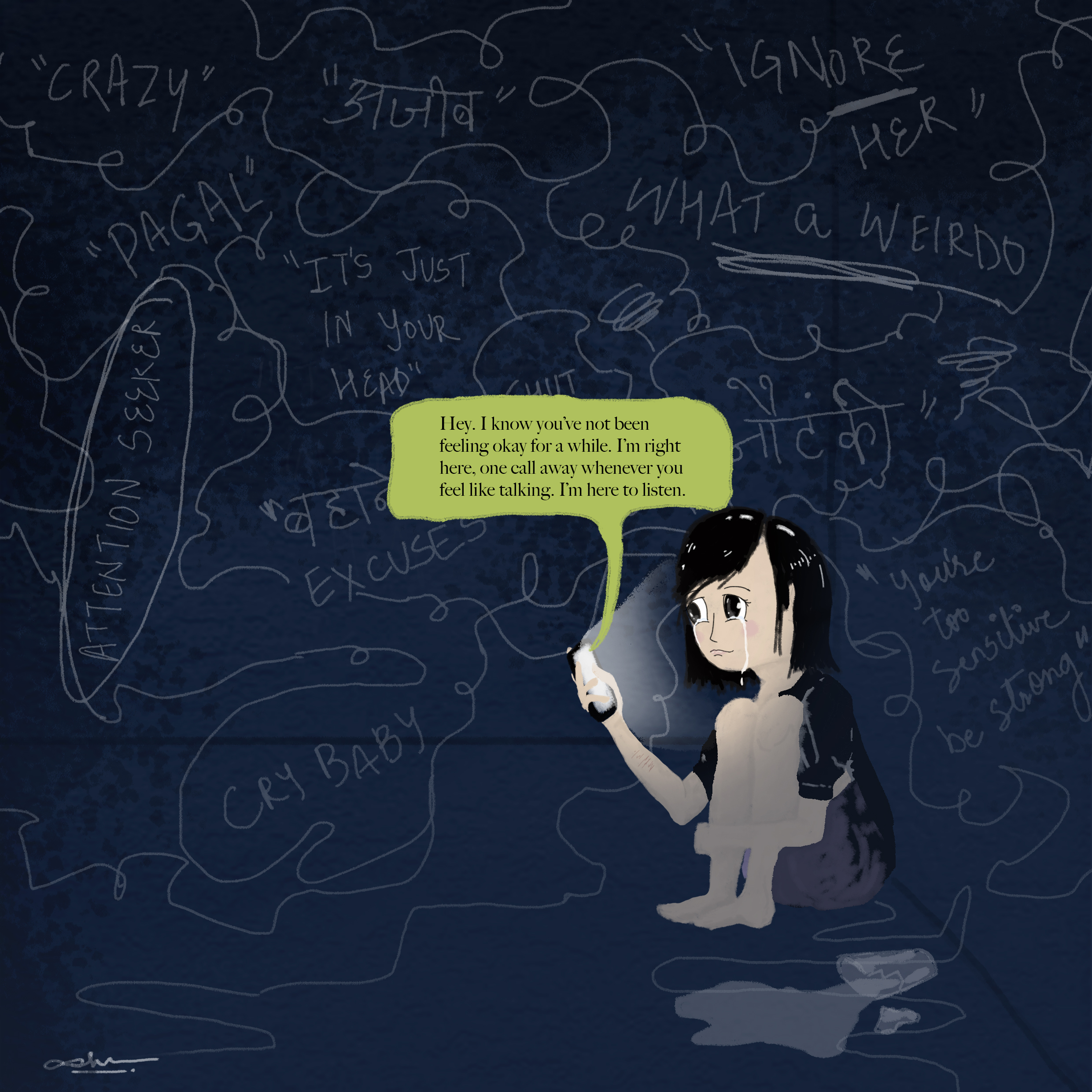
Amongst the many barriers to accessing mental health care, such as the low priority given to mental health by policy makers, the current organization of mental health services which includes lack of integration within primary care, inadequate human resources for mental health; lack of awareness is one of the most important and easily remediable factors. This lack of awareness about the availability, safety and efficacy of psychiatric treatment is rampant not only amongst the lay public but also among the medical professionals.
In India, the low priority given to undergraduate training in psychiatry is of concern. There are very few hours allotted to psychiatry teaching and that too is not taken seriously, chiefly because psychiatry does not find a place in university examinations. If psychiatry gets its due in the MBBS curriculum, the treatment gap may be reduced substantially. Improving undergraduate training is a long term objective. Meanwhile, it is of great importance for the medical fraternity to join hands and clear some myths related to treatment of psychiatric illnesses.
Firstly, the treatment outcomes of mental illnesses compare favorably with treatment outcomes of most non-communicable diseases. Secondly, contrary to popular belief, most psychotropics are safe. In fact, most psychotropics have a larger therapeutic index than many commonly used medications like anti-diabetics, anti-hypertensives etc. Another commonly held view is that psychotropics are habit forming. While it is true that some mental illnesses require long-term treatment, but barring benzodiazepines, psychotropics are just as habit forming as anti-hypertensives. The body needs some of them for proper functioning under certain conditions.
As medical professionals, we could contribute a large deal by identifying mental health problems in our clinical practice and in our interactions with friends, family and society and educating them that treatment of mental illnesses is available, safe, effective and not habit forming. This small endeavor will go a long way in achieving MENTAL HEALTH FOR ALL.

Department of Psychiatry, PGIMS, Rohtak, Haryana
Email: nikhil.jain.psych@gmail.com